The use of magic mushrooms, or psilocybin-containing fungi, in medicine is not a new concept, but its reemergence in the modern medical landscape signals an exciting shift. For centuries, indigenous cultures in Central and South America have used psilocybin for spiritual and healing purposes. In the mid-20th century, scientists began to explore its potential therapeutic applications, but the war on drugs halted much of the progress. Now, with a growing body of research indicating the profound benefits of psilocybin, Canada is positioning itself as a leader in psychedelic medicine.
As public perception of psychedelics becomes more positive and scientific studies continue to showcase their potential, Canadian regulators, medical professionals, and investors are taking notice. Psilocybin therapy, once considered fringe, is entering mainstream discussions around mental health treatment. This article will explore the current state of psilocybin research, the legal landscape, the potential medical benefits, and the challenges that lie ahead for this burgeoning field in Canada.
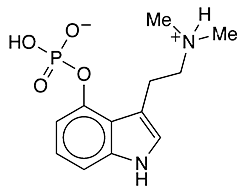
The Science Behind Psilocybin: Understanding the Compound
Psilocybin is a naturally occurring psychedelic compound found in over 180 species of mushrooms. When ingested, psilocybin is converted by the body into psilocin, which interacts with serotonin receptors in the brain. Specifically, it binds to serotonin 2A receptors, which are responsible for modulating mood, cognition, and perception.
The effects of psilocybin can include altered sensory perceptions, profound changes in thought patterns, emotional breakthroughs, and in some cases, mystical or spiritual experiences. While the psychedelic “trip” itself is of interest, it is the compound’s therapeutic potential in mental health treatments that is driving the current resurgence of interest.
Key Areas of Psilocybin Research:
- Mental Health Treatment: Psilocybin is currently being researched for its potential to treat a variety of mental health disorders, including depression, anxiety, post-traumatic stress disorder (PTSD), and addiction. Preliminary studies have shown promising results, particularly for treatment-resistant depression, where other medications have failed.
- Neuroplasticity: Early research suggests that psilocybin may promote neuroplasticity—the brain’s ability to form new connections and adapt to new information. This could be a key mechanism by which psilocybin helps treat mental health conditions, allowing the brain to “rewire” negative thought patterns.
- Spiritual and Mystical Experiences: Many patients report that a single psilocybin session offers a profound, life-changing experience. For some, this has helped with existential anxiety, particularly for those facing terminal illness.
- Cluster Headaches and Chronic Pain: Beyond mental health, psilocybin is also being explored for its potential to treat chronic pain conditions, including cluster headaches. Though research is still in its infancy, anecdotal evidence and early clinical trials are encouraging.
While the scientific mechanisms of psilocybin are still being explored, the consensus is clear: this compound has immense potential. As studies continue to uncover new therapeutic applications, the need for a legal and medical framework to support its use becomes even more critical.
Legal Landscape: Psilocybin’s Regulatory Journey in Canada
Psilocybin is currently classified as a Schedule III substance under Canada’s Controlled Drugs and Substances Act (CDSA). This makes it illegal to possess, sell, or distribute psilocybin without proper authorization. However, recent developments suggest that this may be changing.
Key Legal Milestones:
- Section 56 Exemptions: In August 2020, the Canadian government granted several terminally ill patients Section 56 exemptions under the CDSA, allowing them to legally use psilocybin for end-of-life care. This was a groundbreaking moment in Canada’s legal history, marking the first time in decades that individuals had been granted legal access to psychedelics. Following this, a number of exemptions were also granted to healthcare professionals who wished to use psilocybin in their own therapeutic practices.
- Special Access Program (SAP): In January 2022, Health Canada made a significant policy change by allowing physicians to apply for psilocybin therapy through the Special Access Program (SAP). The SAP was originally designed to grant patients access to unapproved treatments in cases of serious or life-threatening conditions when conventional therapies have failed. This move signals a step towards wider acceptance of psilocybin in medical settings, though it still falls short of full legalization.
- Decriminalization Efforts: Several cities in North America, including Vancouver, have seen grassroots efforts to decriminalize magic mushrooms. In Vancouver, while psilocybin remains technically illegal, enforcement has been lax, with businesses openly selling microdoses of the compound. This echoes similar efforts in the U.S., where cities like Denver and Oakland have decriminalized psychedelic plants.
- Ongoing Clinical Trials: Legal progress is also closely tied to clinical research. Canada has become a hotspot for psilocybin research, with numerous universities and research institutions conducting clinical trials. These studies are crucial not only for proving psilocybin’s efficacy but also for shaping future regulations. With positive clinical results, lawmakers will likely face increasing pressure to loosen restrictions on psilocybin.
The Road Ahead:
While recent developments are promising, there are still significant legal hurdles to overcome before psilocybin is widely accessible in Canada. Critics argue that the current framework is too restrictive, limiting access to only a small group of patients. However, advocates point to the rapid pace of change in both policy and public opinion. As more Canadians become aware of the benefits of psilocybin, the push for broader decriminalization or medical legalization will likely intensify.
Medical Applications: Psilocybin’s Role in Treating Mental Health Disorders
One of the most exciting areas of psilocybin research is its potential to revolutionize the treatment of mental health disorders. As Canada faces a growing mental health crisis, with rising rates of depression, anxiety, and substance use disorders, psilocybin could provide a much-needed alternative to traditional treatments like antidepressants and talk therapy.
1. Treatment-Resistant Depression:
Psilocybin has shown particular promise in treating individuals with treatment-resistant depression. Conventional antidepressants often take weeks or months to show any effects and may come with a host of side effects. In contrast, clinical trials suggest that a single dose of psilocybin, administered in a therapeutic setting, can lead to rapid and lasting improvements in mood.
A 2020 study published in JAMA Psychiatry found that two doses of psilocybin, combined with psychotherapy, significantly reduced symptoms of depression in patients, with effects lasting up to a month. Some patients even reported feeling relief from their symptoms after just one session, a stark contrast to the long-term commitment required for conventional treatments.
2. Anxiety and End-of-Life Care:
For individuals facing terminal illnesses, psilocybin has emerged as a potential tool to help manage end-of-life anxiety. Studies conducted at institutions like Johns Hopkins University have found that psilocybin-assisted therapy can help patients come to terms with their diagnosis, reduce existential distress, and improve overall well-being.
Canada’s Section 56 exemptions have allowed some terminally ill patients to access psilocybin, paving the way for more widespread use in palliative care. For these patients, the compound provides not just symptom relief but also a deeply spiritual experience that can reshape their understanding of life and death.
3. Addiction Treatment:
Psilocybin is also being explored as a treatment for addiction, particularly in cases where traditional therapies have failed. Research has shown that psilocybin can help reset the brain’s reward system, making it easier for individuals to break free from addictive behaviors. Early studies on smoking cessation and alcohol dependence have shown promising results, with many patients reporting a reduced craving for substances following psilocybin therapy.
One theory is that psilocybin’s ability to promote neuroplasticity allows individuals to break free from entrenched patterns of addiction. In addition, the profound emotional and spiritual experiences that often accompany psilocybin sessions can provide patients with the motivation and insight needed to pursue long-term recovery.
4. PTSD and Trauma Therapy:
Another area where psilocybin holds promise is in the treatment of post-traumatic stress disorder (PTSD). Traditional treatments for PTSD, such as cognitive-behavioral therapy (CBT) and antidepressants, often fall short, leaving many patients struggling with debilitating symptoms.
Preliminary studies have shown that psilocybin may help patients process traumatic memories in a way that reduces their emotional impact. By creating a sense of psychological distance from the trauma, patients are better able to confront and resolve their pain. Moreover, the lasting emotional insights gained during psilocybin therapy can contribute to long-term healing.
Challenges and Ethical Considerations
Despite the promising potential of psilocybin, its integration into modern medicine is not without challenges. From regulatory hurdles to ethical concerns, the road to widespread acceptance and use of magic mushrooms in medicine will be complex.
1. Access and Equity:
One of the most significant challenges is ensuring equitable access to psilocybin therapy. Currently, only a small number of Canadians have legal access to the compound through exemptions or special programs. If psilocybin becomes widely available, there are concerns about cost, accessibility in rural or underserved areas, and whether it will be covered by health insurance.
Additionally, psilocybin therapy requires careful administration in a controlled environment, typically alongside psychotherapy. This combination of medical and psychological support can be expensive, further limiting access for marginalized populations.
2. The Risk of Over-Commercialization:
As the psilocybin industry grows, there are concerns about the commodification of a traditionally sacred and therapeutic substance. While pharmaceutical companies are eager to capitalize on the potential of psychedelic therapies, some advocates worry that the focus on profit could overshadow patient care. There is also the potential for “quick-fix” solutions that prioritize convenience over the transformative and sometimes difficult work that psilocybin therapy entails.
3. Safety and Efficacy:
Though psilocybin has shown remarkable safety in clinical trials, it is not without risks. The psychedelic experience can be overwhelming for some individuals, leading to challenging or distressing trips. For this reason, it is essential that psilocybin is administered in a controlled setting, with trained professionals to guide the experience.
Furthermore, while early research is promising, there is still much to learn about the long-term effects of psilocybin, especially with repeated use. Questions remain about how best to integrate psilocybin therapy into existing mental health treatments and whether it is suitable for all patients.
4. Cultural and Spiritual Concerns:
For many indigenous cultures, psilocybin has been used for centuries in spiritual and healing practices. As psilocybin becomes more mainstream, there is concern that these traditions may be co-opted or commercialized without proper respect for their cultural significance. Ensuring that indigenous communities are included in the conversation around psilocybin legalization and research will be crucial moving forward.

The Future Outlook: Psilocybin’s Path in Canadian Medicine
The future of psilocybin in Canadian medicine is bright, but the path forward will require careful planning, research, and collaboration between regulators, healthcare professionals, and the public.
1. Ongoing Clinical Trials:
The next few years will be crucial as ongoing clinical trials continue to explore psilocybin’s efficacy for various mental health conditions. These trials will provide the data needed to support regulatory changes and demonstrate that psilocybin is a safe and effective treatment option.
2. Legal Reform:
With growing public support for psychedelic medicine and positive research outcomes, Canada may see broader legal reforms in the coming years. Decriminalization efforts in cities like Vancouver could pave the way for national discussions about psilocybin’s medical potential. At the same time, expanded access through the Special Access Program will likely lead to greater awareness and demand for psilocybin therapy.
3. Integration into Mental Health Care:
As psilocybin therapy gains acceptance, it could become an integral part of Canada’s mental health care system. Already, some experts are predicting that psilocybin-assisted therapy could help address the country’s mental health crisis by offering new hope to patients who have not responded to traditional treatments.
4. Global Influence:
Canada is positioning itself as a global leader in psychedelic medicine. As more countries explore the medical potential of psilocybin, Canada’s approach to regulation and research could serve as a model for others. By balancing innovation with caution, Canada has the opportunity to set the standard for safe and effective psilocybin therapy.
Conclusion
The future of magic mushrooms in medicine is filled with promise. As Canada continues to explore the therapeutic potential of psilocybin, it is clear that this compound could revolutionize the treatment of mental health disorders, providing relief for patients with treatment-resistant conditions. However, the road ahead is not without challenges. Regulatory changes, ethical considerations, and issues of access will need to be addressed as psilocybin moves into the mainstream.
Canada is at the forefront of this psychedelic renaissance, leading the way with progressive policies, groundbreaking research, and a growing acceptance of alternative treatments. As the stigma surrounding psychedelics fades and the scientific evidence grows, psilocybin may soon become a cornerstone of modern medicine, offering new hope for those in need of healing.
The journey towards widespread psilocybin use in Canadian medicine is just beginning, but the potential is vast. With continued research, collaboration, and ethical stewardship, magic mushrooms could play a transformative role in the future of mental health care in Canada.