Introduction
One of the questions our team here receives more frequently than almost any other about the potential uses for magic mushrooms is: can they help me quit smoking? There has actually been quite a lot of research done around this subject, and although the results are still preliminary, and there’s a lot of additional supplemental research that needs to be done, the early results are quite promising. In the content of this post, we’re going to provide a little background context to smoking and nicotine addiction in Canada, discuss the results of some of the most prominent studies that have been conducted on psilocybin and addiction, and conclude with our own recommendations as to how you might be able to use psilocybin to help you out in your own battle with addiction.
Smoking in Canada
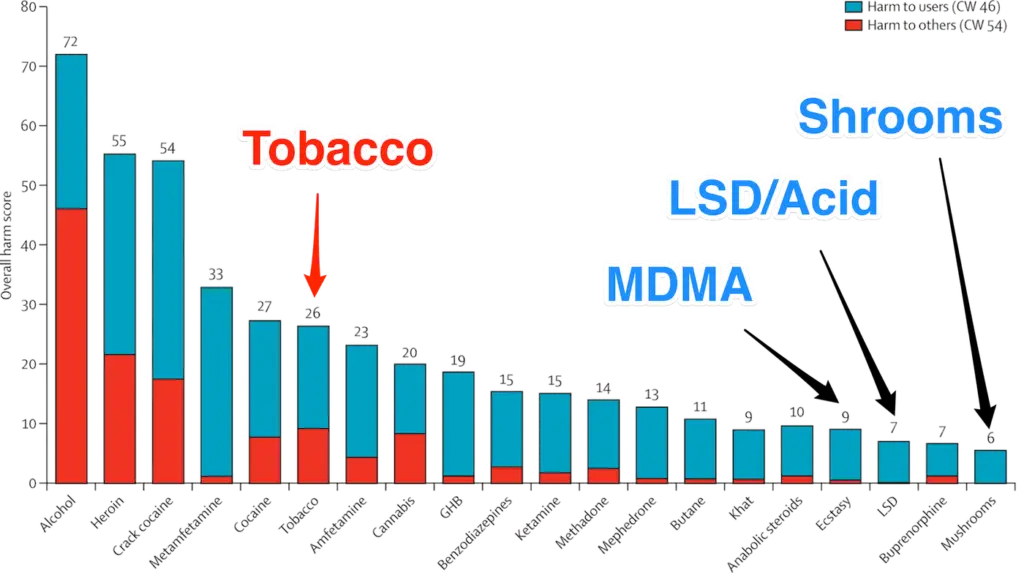
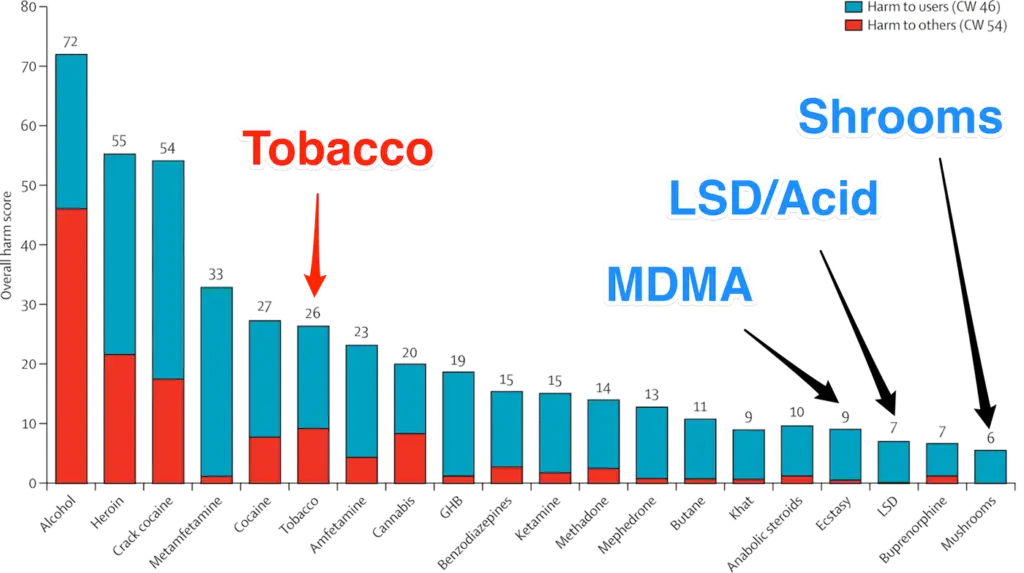
It is certainly no secret that smoking is bad for you – but it still remains one of the most popular addictive substances across the country. In 2015, Statistics Canada published a stunning statistic that 13% of Canadians aged 15 and over smoke tobacco. Smoking is connected with a wide array of different cardiovascular and respiratory diseases and is to this day considered to be the leading cause of preventable death in the country, with 100 Canadians dying every day from a smoking-related illness. Smoking is responsible for about 30% of all cancer deaths, and 85% of lung cancer cases in Canada. Smoking contains highly dangerous carcinogens which can adversely affect the body in a number of ways. Furthermore, smoking is an activity that is increasingly being restricted by Canadian lawmakers. Lawmakers across the country have continued to restrict where smoking is allowed – in 2008, British Columbia banned smoking in all public spaces and workplaces, for example. Other provinces have almost unilaterally followed suit; smokers are increasingly finding themselves with fewer and fewer places in which they can actually smoke, and in 2019, Ontario introduced new legislation that would seek to punish those littering cigarette butts with much higher fines. So, we know that smoking is bad for us, and we know that the government is increasingly taking away the space to do it, and there are fewer and fewer depictions of smoking as a “cool” activity in popular media, and the general perception of smoking being “cool” is rapidly declining as well. One 2016 study found that 80% of people polled thought smoking did not look cool – and this number is continuing to climb. Additionally, the Truth Initiative published a report in which they show that over 70% of smokers want to quit. So, what’s the deal? We know it’s bad, it’s expensive, most people don’t like it, and we want to quit. The Canadian government is even actively funding a multitude of different smoking cessation programs across the country, giving smokers access to free resources including Nicorette gum and patches. So, why are so many people still smoking?
Why Is Smoking So Hard to Give Up?
Well, I think we all more-or-less know why this is the case as well. Tobacco contains the chemical nicotine, which is a central nervous system stimulant that triggers the release of dopamine when it’s absorbed into the bloodstream. And nicotine is one of the most addictive substances on the planet. “From a scientific standpoint, nicotine is just as hard, or harder, to quit than heroin … but people don’t recognize that,” says Dr. Neil Benowitz, a nicotine researcher at the University of California, San Francisco. “Every drug of abuse, including nicotine, releases dopamine, which makes it pleasurable to use,” said Benowitz. “And when you stop smoking, you have a deficiency of dopamine release, which causes a state of dysphoria: you feel anxious or depressed.” Gary A. Giovino, a nicotine researcher at the State University of New York at Buffalo, said as helpful as medication can be, people who really want to quit smoking also have to be willing to modify their lifestyle.
“People need to focus on behavioral change … they need the right skills and knowledge and social support. They need a plan,” said Giovino, a professor and chair of his school’s Department of Community Health and Health Behavior, who quit smoking 40 years ago.
Giovino said good nutrition may be an important factor in helping people quit. He hopes to launch a study that will look at whether there is a correlation between smokers’ vitamin D levels and their ability to stop smoking. He said he’d also like to see researchers explore whether plant-based diets, B vitamins and hydration impact nicotine addiction.
Giovino advises people to tap into the “mind-body connection” and try yoga and deep breathing techniques to help them quit. “After a meal, instead of taking a long breath on a cigarette, (a smoker could) try taking a long, deep breath and exhale without the 7,000 chemicals,” he said.
It’s also important for those who have decided to quit to prepare themselves for how difficult it will be, says Giovino.
“There’s this real roller-coaster ride of not feeling well and being irritable and having cravings,” he said. “The first few days might be very intense, then it might level off and come back again. But the longer you’re off cigarettes, the more your brain goes through the process of neural adaptation, the more you recover. And eventually, the ride subsides.” And yet still, more than 80% of people who attempt to quit smoking will relapse. So where does psilocybin factor into all of this? Well, here’s where we come to the part of the article focusing on the new research emerging that indicates that psilocybin might be able to help many people in their efforts to quit.
Psilocybin Therapy Helps Create a Lasting Change
In 2016, a team of researchers led by Albert Garcia Romeau, PhD, published an article online in the American Journal of Drug and Alcohol Abuse which detailed the summaries of their findings using psilocybin-assisted cognitive behavioral therapy to help chronic smokers kick the habit. A grand total of 15 daily smokers participated in the experiment, which consisted of 2-3 sessions of psilocybin-assisted therapy. These participants were paired with trained therapists who used the time with their patients to create a “mystical” experience in which the patients were guided through a psilocybin-induced high with a focus on helping them abstain from smoking over the long term.
Researchers were attempting to beat the average results that have been achieved in clinical studies not involving psilocybin. As of the time of the study, the most effective smoking cessation studies that had only shown about a 35% rate of success in graduates remaining abstinent after a period of six months. Romeau and co. were interested in seeing whether they could beat those numbers through psilocybin therapy, and the results were incredibly encouraging. Participants were relatively well educated, with all individuals reporting some college, and 11 (73.3%) having received at least a Bachelor’s degree. The sample was racially homogeneous, including 14 (93%) White participants and 1 (7%) Asian participant.
This study was approved by the Johns Hopkins University School of Medicine Institutional Review Board, and all participants provided informed consent. Participants underwent a 15-week smoking cessation treatment intervention, with moderate (20mg/70kg) and high (30mg/70kg) dose psilocybin sessions occurring in weeks 5, and 7 respectively, and an optional third high dose session in week 13. The intervention consisted of weekly meetings for 15 weeks and was delivered by a team of 2 to 3 facilitators. The Target-Quit Date (TQD) was set for week 5 of treatment, concurrent with the first psilocybin session. Afterward, study treatment facilitators met weekly with participants to discuss psilocybin session experiences, encourage and socially reinforce the use of CBT techniques, and provide support for smoking abstinence.
Although definitive conclusions about the role of psilocybin in this study’s smoking cessation outcomes cannot be drawn due to the open-label design and lack of control group, the mystical-type qualities of psilocybin sessions (measured the same day), as well as their personal meaning, spiritual significance, and impact on well-being (measured 7 days after these experiences) are significantly correlated with measures of smoking cessation treatment outcomes at 6-month follow-up. Furthermore, the intensity of psilocybin session experiences was not significantly associated with smoking cessation treatment outcomes, suggesting that mystical-type effects specifically, rather than the general intensity of subjective drug effects, are associated with long-term abstinence.
In other words, even those participants who didn’t indicate that their psilocybin experiences were especially “mystical” or life-changing showed similarly boosted rates in maintained abstinence from smoking. The results from the 6-month follow-up indicated that 12 of the 15 participants (80%) remained smoke-free for 180 days after the conclusion of the treatment. Although the research is preliminary, the sample size is small and there was no control group, it is certainly promising that this small study revealed that people were more than twice as likely to be successful in quitting smoking when assisted through psilocybin therapy as opposed to conventional non-psychedelic treatment.
A Qualitative Analysis of Psilocybin-Assisted Smoking Cessation Programs
In 2018, a team of researchers led by Tehseen Nohri published a paper in the Journal of Psychopharmacology which aimed to consolidate the findings of a wide number of studies conducted a qualitative analysis into the use of psilocybin in smoking cessation programs. So, the idea here is, through interviewing people who had participated in previous smoking cessation studies, to get a better idea as to exactly how magic mushrooms helped them quit smoking, in their own words. These results were separated into a few categories, and the findings are quite interesting.
Insights into Self-Identity
Many respondents reported valuable insights into their understanding of themselves occurring during their psilocybin experiences that were directly relevant to their efforts to quit smoking. Session experiences were described as revealing a deeper, better, or more essential self that either led to a decreased desire to smoke, or to smoking not making sense anymore. One participant said,
“I used to hide sitting on the air conditioning unit on the side of my house when I used to smoke. And so the image was me sitting there, smoking, all hunched over, stupid, smoking. And the vine just rising up and this purply flower face thing looking down at me like, ‘how ridiculous!’ And then I’m not really that [person], I’m really this vine, that’s really me, and the Goddess within me…how silly to think that [smoking]… was going to do anything or solve anything. So it was really just that rising up feeling, and that powerful feeling, and it just filled me with such beauty and strength and life.”
And another shared that,
“It felt like I’d died as a smoker and was resurrected as a nonsmoker. Because it’s my perception of myself, and that’s how I felt. So I jumped up and I said ‘I’m not a smoker anymore, it’s all done.”
Insights into Smoking Behavior
Many participants also reported specific smoking-related insights during psilocybin sessions that they perceived as helpful for quitting. Here’s some of what they had to say: One participant noted the realization that smoking even one cigarette entailed an ongoing commitment to smoking. A specific image from her first session led them to the insight that to smoke at all was to be ‘a smoker’:
“It was me in the red coat, lighting up a cigarette, and then it spread into a grid. So it was like that one cigarette was 1000 cigarettes.”
Similarly, another participant explained,
“Cigarettes don’t seem like a short-term solution anymore. They seem exhausting to me. Like…oh my god – just, having a cigarette now and opening up this whole thing all over again?! To have one cigarette would be a long-term commitment.”
Experiences of Interconnectedness
Many participants described experiencing a profound sense of unity and interconnectedness during their psilocybin session experiences. One had this to say:
“I had always had the sense of everything being connected. And [the psilocybin session] reinforced that, very strongly… [If I were to smoke] I would be a polluter…ashtrays and butts all over the place, and you’re causing harm to other people’s health as well. And so you were re-looking at your place in the universe and what you were doing to help or hinder it. The universe as such. And by smoking, you wouldn’t be helping.”
Sustained Feelings of Awe and Curiosity
Many participants reported that the profound significance of the psilocybin session experiences made smoking seem trivial in comparison. These participants described psilocybin sessions as evoking a powerful, sustained sense of awe and a lingering curiosity into unsolvable life mysteries, all of which diminished the relative importance of smoking. One participant described his experience as…
“…beyond what I have ever been to or any place I ever thought about going to…I was just totally inundated, mentally and emotionally, by that experience. So the smoking was like, ‘who cares!’, you know? Somewhere that’s so special and so unique and it’s shown me so much in such a brief period of time…[after that] smoking is not important anymore!”
Reduced Withdrawal and Cravings
The first psilocybin session was followed by a marked reduction in the reported intensity and frequency of withdrawal symptoms for 91% of the participants when compared with their previous experiences attempting to quit smoking. These individuals went on to maintain abstinence between their first and second psilocybin sessions.
Closing Thoughts: How to Use Magic Mushrooms to Help you Quit
Of course, as with any time we create a post that discusses a mental health condition such as addiction, we need to include the caveat that the safest way to engage in any of this is to consult directly with a physician or therapist before taking anything on. However, for those who are looking to take this on themselves, we do have some specific recommendations.
1: Have Clear Intentions
We’re beginning to feel a bit like a broken record, constantly repeating this one piece of advice – but it holds true in this case especially. If you’re looking to use magic mushrooms as a way to help you quit smoking, keep your intentions clear and pure in your head before you take your dose. If your intentions aren’t clear going into a trip, it can be easier to become distracted and miss the insights you might have gained by remaining focused on your goal.
2: Do it for You
Anecdotally, we’ve heard stories about people who’ve tried to use mushrooms to help them quit because of pressure from a family member or friend, instead of for their own reasons. Almost invariably, we’ve found that these people have less success with quitting than those who are doing it for their own reasons. Like we mentioned at the beginning of the article, smoking is bad for you! It’s expensive, addictive, and harmful. There are plenty of great reasons why any smoker should want to quit the habit for their own benefit, and you’re going to get a much more lasting effect from the experience if you’re doing it for your own reasons and not for someone else’s.
3: Be Humble
It’s important that, if you’re going into this with the idea that you’ll get some kind of benefit out of it, you go into it with some humility. The entire concept is based around the idea that the mushrooms will give you some kind of insight that is not alien to you, but which you have not been able to access before. It is likely that you will experience insights or ideas that run counter to ideas that have been ingrained in you for some time, and it requires humility to welcome these ideas. Keep your goal of quitting smoking front of mind, and be willing to accept the novel ideas that come to you in support of this goal.
4: Use a Trusted Source
It is of absolute importance that you use a trusted source when attempting to take magic mushrooms for any reason, but especially when looking for magic mushrooms for therapy. Of course, we would be happy to help – you can buy shrooms online here!
4: Document your Experience
This is another constant piece of advice that we offer to anyone who is looking to use mushrooms for purposes related to self-improvement, or mental health. Take note of what it is that you’re feeling – this could be by writing it down, or even simply through conversations with a friend. Notice how you feel about smoking while you’re under the influence of the mushrooms, notice how you feel as the effects wear off, and days and weeks after.