Magic mushrooms were once a counterculture symbol. Today, they’re on the cutting edge of mental health care. What was dismissed as psychedelic escapism is now being studied in labs, trialed in hospitals, and prescribed in select clinics around the world.
At the heart of this shift is psilocybin, the naturally occurring psychedelic compound found in over 180 mushroom species. Researchers have shown that psilocybin, especially when paired with psychotherapy, may treat some of the most stubborn and devastating mental health disorders—depression, anxiety, PTSD, addiction, and even existential distress in terminal illness.
This isn’t hype. This is what the data now says. This blog breaks down how psilocybin works, where it’s being tested, what studies from 2024–2025 reveal, and what it all means for the future of mental health.

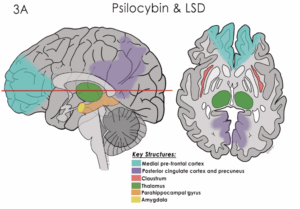
How Psilocybin Works in the Brain
Psilocybin is converted in the body to psilocin, which binds to serotonin receptors in the brain—particularly 5-HT2A receptors. These receptors play a major role in mood regulation and perception. But psilocybin does more than tweak your serotonin levels—it appears to reset the brain’s default mode network.
What’s the default mode network (DMN)? It’s the part of the brain responsible for self-reflection, rumination, and our sense of ego. In depression, the DMN becomes overactive and rigid. Psilocybin loosens this grip, increasing neural connectivity and allowing for emotional “unfreezing.”
Studies using fMRI scans show that after a psilocybin session, the brain exhibits greater cross-talk between regions, leading to heightened emotional insight and plasticity. Patients often report not just feeling different—but thinking differently.
Psilocybin and Depression: The Hard Numbers
Depression and Treatment-Resistant Cases
In 2025, the largest study of psilocybin for major depressive disorder published its findings: patients who received a single 25mg dose—administered with professional therapeutic support—experienced a statistically significant reduction in depression scores compared to those who received a placebo.
While the margin wasn’t as large as early studies suggested, 40–50% of participants reported sustained relief at one month, with some maintaining improvement for a year or more. That’s remarkable for a single dose of a non-daily medication.
Compass Pathways, a biotech company leading this research, also revealed that psilocybin’s effect outpaced most conventional antidepressants—but with far fewer side effects and a unique mechanism of action.
Cancer-Related Depression and Anxiety
Terminal illness brings not only physical pain, but deep existential despair. Traditional antidepressants can dull this pain, but they rarely bring peace. Psilocybin seems to.
NYU Langone researchers ran a study with cancer patients facing end-of-life anxiety and depression. A single 25mg psilocybin session, paired with psychotherapy, led to immediate relief—and in 2025 follow-ups, over 50% of participants were still symptom-free after two years.
These patients weren’t just “less anxious.” Many described the experience as life-altering—feeling “at peace,” “connected,” or “unafraid of dying.” For some, it was the most meaningful event of their life.
Beyond Depression: Addiction, OCD, and Trauma
Alcohol and Substance Use Disorders
Addiction rewires the brain’s reward systems. Psilocybin appears to help rewire them back. In a 2024 study out of NYU, patients with alcohol use disorder who received psilocybin-assisted therapy reduced their drinking days by over 80%, with sustained improvements at the one-year mark.
These results echo early findings on tobacco addiction, cocaine cravings, and even opioid use. Psilocybin doesn’t act like methadone or nicotine patches. Instead, it changes how patients relate to their cravings, often triggering profound personal insights and new motivation.
Obsessive-Compulsive Disorder (OCD)
Although smaller in scale, studies on OCD show promise. Psilocybin appears to disrupt repetitive thought loops and compulsions, allowing patients to step back from intrusive thoughts. In one trial, nearly 60% of participants reported a significant drop in OCD symptoms after two sessions.
Microdosing and Novel Treatments
Microdosing
While full-dose psilocybin therapy is conducted under clinical supervision, microdosing—taking sub-perceptual amounts of psilocybin (usually ~0.1–0.3g)—has taken off among the general public. Users claim increased focus, mood stability, creativity, and emotional resilience.
However, scientific validation has lagged behind. A few 2024 trials did find that microdosing improved mood and stress tolerance compared to placebo—but the effects were modest. Importantly, microdosing appears to carry low risk of dependency or toxicity, but standardization remains a challenge due to variation in mushroom potency.
IV Psilocybin: The TRP-8803 Trial
One of the most cutting-edge developments in 2025 is the IV psilocin drip trial in Australia. The treatment, known as TRP-8803, delivers precise, steady amounts of psilocin (the active form of psilocybin) through an intravenous system. This allows for faster onset, easier dosage control, and potentially lower risk of adverse reactions.
Early applications are focused on binge-eating disorder, where emotional regulation and impulsivity play a key role. If successful, IV psilocybin could open the door to scalable treatment models that don’t require six-hour trips in a therapist’s office.
Real People, Real Stories
From the Field: Rory Lamont and Athlete Recovery
Former Scotland rugby player Rory Lamont described battling years of depression and PTSD after leaving professional sport. Conventional therapy failed. Psilocybin, alongside other plant medicines like iboga, helped him process buried trauma and restore emotional health.
Lamont’s story underscores the potential power—and the risks—of psychedelic self-treatment. Experts warn that such experiences should only happen under careful supervision to avoid psychological distress or retraumatization.
The Banker’s Journey
Australian banker Joseph Healy paid over $5,000 for a legal psilocybin experience in the Netherlands. He came back feeling renewed and more emotionally present, describing it as “intense but profoundly healing.” He’s since launched Malu Health, a company aiming to bring supervised psychedelic therapy to Australia.
What Are the Risks?
Psilocybin is not a miracle cure. It comes with risks—especially when used improperly. The most common side effects are nausea, anxiety, confusion, or distress during the experience. In rare cases, users with personal or family history of psychosis may be at risk for adverse psychological outcomes.
Experts stress the importance of set and setting: your mindset, the environment, and whether you have trained therapeutic support during the trip all shape the outcome. Bad trips are not uncommon, but with guidance, they can often become breakthroughs instead of traumas.
Long-term dependency or abuse is rare, but unsupervised use—especially when used frequently or in combination with other substances—can lead to emotional instability.
The Legal Landscape
The legal status of psilocybin is changing rapidly. Here’s a snapshot as of mid-2025:
-
Australia legalized psychiatrist-prescribed psilocybin therapy for treatment-resistant depression and PTSD in July 2023.
-
Canada allows psilocybin-assisted therapy in Alberta under a regulated medical model.
-
New Zealand has moved toward prescription-only access via registered psychiatrists.
-
In the U.S., Oregon and Colorado now permit therapeutic psilocybin use in licensed centers. Several other states are evaluating similar frameworks.
-
The EU is watching closely. Czech lawmakers are debating a bill to allow clinical access to psilocybin under psychiatric supervision.
Where the Research Is Going
Hundreds of clinical trials are now in motion. Here are some active or upcoming lines of research:
-
Anhedonia (loss of pleasure) in depression and schizophrenia
-
Anorexia nervosa and body dysmorphia
-
Chronic pain and fibromyalgia
-
Parkinson’s-related depression
-
New AI-guided integration tools helping patients process and apply their psilocybin experiences with the aid of digital companions
These are not fringe experiments anymore. They are funded by universities, regulated by health ministries, and scrutinized by ethics boards.
Why It Matters
Mental health care is in crisis. Antidepressant prescriptions are up, but patient outcomes are not. Suicide remains a leading cause of death. Too many people are stuck—untouched by traditional meds, overwhelmed by trauma, or lost in meaninglessness.
Psilocybin doesn’t offer an escape. It offers a reset. A chance to view one’s pain from a different angle. A therapeutic “window” where healing becomes possible.
No, it’s not for everyone. And no, it’s not magic. But it is medicine, and it’s helping people where nothing else could.
Buy The Best Magic Mushrooms in Canada Right To Your Doorstep (19+)
References
-
The Times UK
-
“Magic mushrooms enter mainstream as treatment for depression” (also titled Is psilocybin really a cure for depression?)
→ [Read on The Times UK]
Herald Sun
-
“Magic mushrooms via drip: World‑first experimental therapy revealed”
→ [Read on Herald Sun]
ScienceDaily (Cancer trial)
-
“Single psilocybin trip delivers two years of depression relief…”
→ [Read on ScienceDaily]
NYU Langone Health / ScienceDaily
-
Psilocybin eases existential distress and systemic improvement in cancer and alcohol use disorder
→ [Read on NYU Langone / ScienceDaily]
Compass Pathways (COMP360 study)
-
COMP360 psilocybin therapy for treatment‑resistant depression (phase II/III results)
→ [Read via Compass Pathways / NEJM summary]
UCSF Clinical Trials
-
Active clinical trials with psilocybin in anorexia, Parkinson’s depression, chronic pain
→ [View UCSF psilocybin trial listings]
Wired
-
“People Are Using AI Chatbots to Guide Their Psychedelic Trips”
→ [Read on Wired]
Wikipedia
-
Psychedelic therapy, Psilocybin itself, Psilocybin decriminalization in the U.S.
→ [View on Wikipedia]
-